Acne
Acne is a chronic skin disease involving inflammation of the sebaceous glands. It affects 80% of teenagers and many adults, especially women, 35% being between the ages of 30 and 40. Acne represents 15-20% of all dermatology consultations.
Disease overview
Description
[“ack-nee”]
Acne is a skin disease that is particularly common among adolescents, though some people have acne that lasts into adulthood.
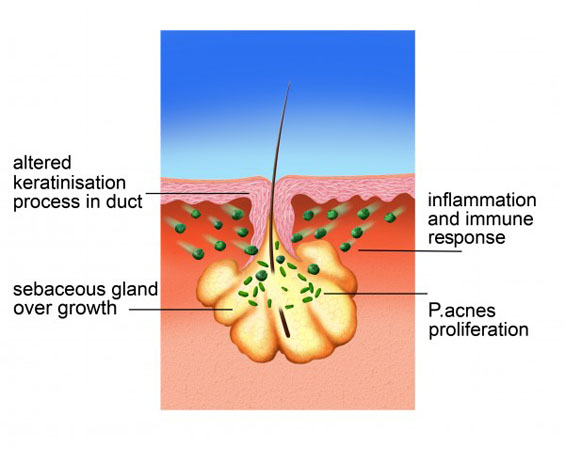
Acne involves a disorder with glands in the skin that are located next to hair follicles. These glands, called sebaceous glands, secrete an oily substance called sebum. Everyone has these glands, and the secretion of sebum is normal, but people with acne have overactive glands that release more sebum in into the skin. At the same time, the dead skin cells lining the pores are not shed properly and, combined with the extra sebum, clog up the follicles. This effect can lead to blackheads (where a darkened plug of oil and dead skin is visible) and whiteheads. Blackheads and whiteheads are together known as comedones.
The acne bacterium, P.acnes, lives naturally on everyone’s skin, but the blocked pores full of excess sebum are a great environment for it to thrive, and so in people with acne it is present in much greater numbers.
All these factors lead to inflammation of the skin and the spots, papules and pustules we associate with acne.
Diagnosis
In most cases, a dermatologist or other healthcare provider can make a diagnosis by examining the affected skin. However, your healthcare professional may ask several questions that are aimed at ensuring a proper acne diagnosis and to rule out other skin disorders. These may include questions about:
- Areas of sensitive skin, or eczema
- Other diseases that may affect the ability to handle medications
- Previous drug allergies
- Use of steroids (e.g. for bodybuilding)
- Mood disorders or depression
- Use of contraceptives, irregular menstrual period, current or past pregnancy, breast feeding
In some cases acne can mimic other related skin disorders, such as rosacea. This information will help your healthcare professional make an informed diagnosis.
Emotional Consequences of Acne
Having acne does not just mean superficial or cosmetic changes to the skin – it can have an emotional aspect to it as well. Since the face is one of the primary areas affected by acne, symptoms of the disease can change the appearance of those affected, and this can lead to stress and anxiety. Depending on the severity of the condition, acne can lead to a negative self-image, including:
- Low self-esteem
- Loss of confidence
- Depression
These emotional consequences affect anyone who is suffering from acne – both men and women, young and old. In addition to reducing the quality of life of people with acne, the emotional aspects of the disease have been shown to reduce productivity and employability. This impact on quality of life is comparable to what is seen in diseases like epilepsy or asthma. There are also several myths surrounding acne, and this can cause misplaced feelings of guilt that worsen the emotional effects of the disease.
Causes, Triggers, and Risk Factors
The exact cause of acne is not known, but researchers think that both genetic and environmental factors play a role. Family history of acne is a risk factor which suggests a genetic component. In addition, there are environmental factors, or “triggers,” that also increase the risk of acne. You may notice that certain factors in your daily life may trigger your acne symptoms and cause pimples to flare up. Triggers can be very different from one person to the next, and it is important for you to keep track of your triggers to help you avoid them and help to minimise ‘flare-ups’.
| Factors that may trigger acne include:Certain medications | Certain steroid medications can cause symptoms very similar to those seen in acne. These symptoms will typically appear suddenly and progress rapidly. Corticosteroids, for example, can induce a characteristic form of acne that does not have comedones (blackheads or whiteheads), but rather papules and pustules. Anabolic steroids can also induce acne, in this case with prominent blackheads and whiteheads on the surface of affected skin. If you feel that a medication you are taking is making your acne worse, mention this to you healthcare professional. |
| Certain cosmetics and skin care products | Many cosmetics contain agents that are noncomedogenic—in other words, these agents don’t plug pores and cause whiteheads or blackheads. However, there are still some cosmetics with comedogenic agents. If you are worried that applying cosmetics or other skin care products is making your acne worse, you can look for labels that specify that these products are “noncomedogenic,” “non-pore-clogging,” or “oil free.” |
| Sweating | There is some indirect evidence that sweating or humid environments may trigger acne. It is possible that excess humidity partially blocks pores, leading to acne. Avoiding excess sweating and humid environments may help keep your pores free of clogging and result in fewer acne symptoms. |
There are also known risk factors for acne. Anyone can develop acne, but these factors can alter your risk of showing symptoms:
| Family history | Hereditary factors seem to play a large role in acne development. This means that if acne runs in your family, you’re more likely to have it yourself. |
| Menstrual period | Many women note that their acne tends to get better and worse in cycles, and that this is related to their menstrual period. Roughly 40% of female patients note acne flare-ups in the days leading up to their period. |
| Pregnancy | Hormonal changes during pregnancy may also result in temporary acne flares. Some treatments for acne, in particular oral isotretinoin, are associated with serious birth defects if used during pregnancy (see types of prescription treatment – below), so it is important to report pregnancy to your dermatologist and to inform your doctor of all acne medications you are taking. |
Diet
Diet has long been a controversial subject in acne research. There is a popular notion that greasy foods somehow contribute to oily or acne-prone skin. However, scientific studies of the causes of acne have not shown this to be true. Researchers have discovered some links between acne and certain components of a “Westernised diet”—specifically high sugar foods and dairy products. However, there is no conclusive evidence for other food items such as chocolate or saturated fats.
KEY MESSAGES:
IMPORTANT FACTS ABOUT ACNE
- Acne is not infectious, and is not caused by poor hygiene
- Whilst acne typically first appears in adolescence, it may persist well into adulthood
- Acne requires short and long-term therapy
- Acne has an emotional side, with many people feeling stress or anxiety about the way it changes their appearance
- There is no conclusive evidence that fatty foods or chocolate are responsible for acne
Treatments & Practical Tips
Below you will find some information on treatments that are available for acne prone skin, as well as considerations and practical tips for patients coping with acne. Speak to your healthcare professional for who will be able to advise the appropriate treatment for you.
Treatments for acne can be very effective at reducing spots and improving the appearance of skin, but this requires time. It is natural to want to see the effects of any treatment right away, but most treatments will not have a significant effect until several weeks have passed. People with acne who experience this can sometimes become frustrated with this delay, and stop taking their medication before it has had time to make an effect on their symptoms. Keep in mind that this is typical of acne treatment, and don’t be discouraged if acne does not improve in the first few days. Also, several treatments for acne may initially make symptoms worse at the start of therapy. This is a temporary effect and sticking with the treatment as directed by your healthcare professional will typically result in symptoms improving after the first few weeks. It’s important to always take acne treatments as prescribed by your healthcare professional and give them the necessary time before making decisions on their effectiveness.
It is important to understand that acne is a long-term disease. Most people’s acne resolves when they are in their twenties. However, some people with acne will have symptoms that stay with them their entire lives. There are several effective treatment options, but no one “cure” for acne. In some cases acne medications should be taken over the long term, as stopping treatment when the acne improves can result in symptoms coming back. In some cases, your healthcare professional may prescribe an initial treatment to get your acne under control, followed by a long-term treatment that can help keep it from coming back.
Types of Prescription Treatment
Acne is a very common disease that significantly affects the lives of people who have it. Fortunately, there are treatments that can help reduce symptoms. This can improve the appearance of the skin, and lead to a better quality of life for people with acne. Acne treatment usually aims to:
- Make existing pimples go away
- Stop new pimples from forming
- Limit side effects to a tolerable level
- Help prevent scarring of the skin when possible
Speak to your healthcare professional who can advise on the most suitable treatment for you.
| Treatment | How it works in acne |
| Topical Retinoids (retinoids for topical use in acne) | Topical retinoids are derivatives of vitamin A. These different treatments have similar abilities to improve acne, but all can irritate the skin, particularly during the first few weeks of use. Topical retinoids can be used as initial treatment and as long-term maintenance therapy. Some topical retinoids can be found in fixed-dose combination products with other topical agents (eg. adapalene and benzoyl peroxide) |
| Benzoyl Peroxide (peroxides, anti-acne for topical use) | Benzoyl peroxide is an antimicrobial, meaning it can kill bacteria. It is able to quickly and effectively kill P. acnes, bacteria in the skin of people with acne. Unlike antibiotics, bacteria have not been able to become resistant to benzoyl peroxide. It is available in several different concentrations. The more concentrated forms may be more irritating to the skin. |
| Topical Antibiotics | Topical antibiotics are able to kill bacteria, including P. acnes . Antibiotics are also able to reduce inflammation in the skin. Unlike benzoyl peroxide, antibiotics are limited by antibiotic resistance. These bacteria may not be affected at all by antibiotics or may become progressively resistant over the course of treatment. To reduce the proliferation of antibiotic-resistant bacteria, antibiotics are often used in combination with other treatments. |
| Oral Antibiotics | Oral antibiotics are antibacterial and anti-inflammatory, but are taken as pills or capsules rather than creams or lotions and are often used in more severe forms of acne. |
| Hormonal / Antiandrogen Therapy | These treatments are options for women with endocrine abnormalities or difficult-to-treat acne. |
| Oral Retinoids (retinoids for treatment of acne = isotretinoin) | Oral isotretinoin acts on the four factors involved in the pathogenesis of acne. It is used for the most severe cases of acne, or in cases where other treatments cause continued relapse or cannot prevent scarring. Women taking oral isotretinoin cannot be pregnant at the time of initiating treatment, and cannot become pregnant during treatment or one month after stopping therapy, due to birth defects caused by the drug. A strict contraception regimen must be followed. |
The Right Treatment for You
Your healthcare professional will help you to decide which treatment is best for you. In addition, you may want to consider the following factors when selecting an acne treatment that is right for you:
- First, the treatment should never be worse than the acne itself.
- The treatment may need to be used for prolonged periods of time or continuously in order to keep acne symptoms under control
- Some acne treatments (particularly oral treatments) are associated with birth defects; if you are pregnant or plan on becoming pregnant during acne treatment it is important to talk to your healthcare professional about what treatment options are appropriate
- Acne treatments may be irritating to the skin and appear to be causing even more acne, but don’t worry if this is the case, use your treatment every other day, use a non-comedogenic moisturiser and call your healthcare professional. These irritations are temporary and generally resolve fairly quickly with continued use of the treatment.
- Keep in mind: treatment adherence strongly influences treatment effectiveness (If you don’t use it, it won’t work!)
Practical Treatment Tips
Cleansing
Cleansing habits are an important aspect of treating acne, but are also an area of misinformation for people with this disease. Keep in mind that acne is not caused by poor hygiene: there is no evidence that a lack of washing causes acne or that frequent washing improves it. In addition, cleansing that is too frequent or too vigorous can actually make matters worse by aggravating the skin. This is especially true if rough cloths or other scrubbing materials are used. These abrasives disrupt the follicle and cause further aggravation to the inflamed skin. The best practice is to clean affected areas using only warm water and a gentle cleanser no more than twice daily. Also, some prescription acne treatments should not be used with harsh cleansers or scrubs because they may increase irritation. Make sure you discuss with your healthcare professional all skin products and cleansers you are using before you start treatment with a prescription product.
The choice of cleanser is also an important consideration. Although P. acnes bacteria play an important role in acne, soaps labelled “antibacterial” have not been found to help. These soaps typically don’t affect P. acnes, in pore (where it causes problems), but can only wash off bacteria from the surface of the skin.
Skin Care Tips
- Clean skin gently. Use a mild cleanser in the morning, evening and after heavy workouts. Scrubbing the skin does not stop acne.and may even make the problem worse.
- Sometimes even acne-prone skin can feel dry (particularly when first using topical medication like retinoids). Using a mild, “non-comedogenic” moisturiser may help, but avoid oily or heavy products that can clog pores.
- Shave carefully. If you shave, you can try both electric and safety razors to see which works best. With safety razors, use a sharp blade. Also, it helps to soften your beard with soap and water before putting on shaving cream. Shave lightly and only when you have to.
- Choose makeup carefully. All makeup should be oil free. Look for the word “non-comedogenic” on the label. This means that the makeup will not clog up your pores.
- Stay out of the sun. Many acne medicines can make people more likely to sunburn.
KEY MESSAGES:
HELPFUL HINT
All topical treatments should be spread over the entire area where acne appears, not “spotted” only on visible pimples. Talk to your healthcare professional about the best way to apply a topical medication.
CAUTION
Try not to touch your skin. People who squeeze, pinch, or pick their spots can get scars or dark spots on their skin.
Lifestyle Measures
People with acne sometimes find that lifestyle measures help improve the appearance and reduce the discomfort of affected skin. These typically involve basic skin care:
| Use a gentle cleanser | § Stay away from facial scrubs, astringents, and masks—they tend to irritate skin, which can make acne worse.
§ Very frequent washing or scrubbing can also irritate skin. |
| Use non-comedogenic skin products | § You may want to avoid oily or greasy cosmetics, hairstyling products or acne concealers.
§ Look for products labelled “water-based” or “non-comedogenic”. |
| Stay out of the sun | § The sun can make acne worse for some people.
§ Acne medications can also make your skin more susceptible to the sun’s rays. § Check with your healthcare professional if your medication could make you more sensitive to the sun, and if so stay out of the sun as much as possible. § If staying out of the sun is unavoidable, use a non-comedogenic sunscreen that won’t clog your pores. |

